Gynaecology
Besides his love for Obstetrics, Dr Deon Van Zyl also has vast experience managing various gynaecological conditions. He uses a conservative approach in the management of gynaecological conditions, opting for medical management over surgical management, where possible.
Your Health First
Besides his love for obstetrics, Dr Van Zyl also has experience managing various gynaecological conditions.
These include, but are not limited to:
Dr Van Zyl tends to be conservative in the management of gynaecological conditions, opting for medical management over surgical management, where possible. However, when medical management fails, or where it's not possible or advisable, surgery is performed endoscopically (keyhole surgery) where possible. This ensures a quicker recovery with less pain and time away from family/work.
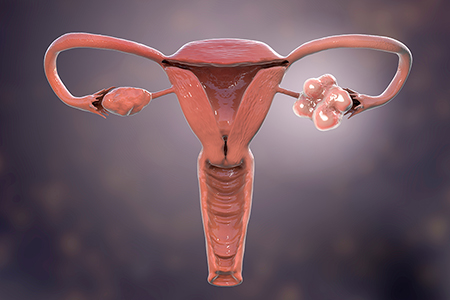
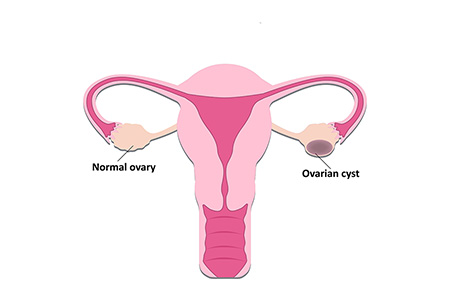
Endoscopy is integral to surgery in modern gynaecology. Dr Van Zyl practices advanced laparoscopic and hysteroscopic surgery for conditions including severe endometriosis, fertility, cysts, fibroids, uterine abnormalities, prolapse repair and hysterectomy. In addition, vulval and vaginal surgery allows the correction of prolapsing tissues, treatment of urinary stress incontinence, and labial reduction.
Frequently Asked Questions
The simple answer is to pursue egg freezing, or oocyte cryopreservation, in the prime reproductive years — a woman's 20s and early 30s — to take advantage of premium egg quality and quantity. A woman is born with all the eggs she will ever have, and over time they diminish in number and cellular integrity. This decline explains why a woman in her 40s has only a 5% chance of becoming pregnant each month, and her eggs have an increased chance for aneuploidy after age 45.
Basic fertility testing, including antral follicle counts, hormone and AMH blood testing, assesses your ovarian reserve. A clearer picture of your egg quantity and ovarian function may lead you to opt-in (or out) of elective fertility preservation. Life circumstances may also lead you to consider egg freezing. For some women, knowing that they have preserved eggs brings them peace of mind in a season of life inconsistent with pregnancy. For example, women with demanding careers or the inflexibility of academic calendars may wish to delay family building.
The majority of women with PCOS will have insulin resistance. This usually leads to increased weight and difficulty in losing said weight. Therefore, weight loss, which can restore ovulatory cycles and improve metabolic risk, is the first-line intervention for most women. The approach to obesity management is the same as that for patients without PCOS, starting with lifestyle changes (diet and exercise), followed by pharmacotherapy and, when necessary, bariatric surgery.
We suggest weight-loss strategies using calorie-restricted diets combined with exercise for women with PCOS and obesity. Even modest weight loss (5-10% reduction in body weight) in women with PCOS may restore regular ovulatory cycles and improve pregnancy rates in short-term studies. However, the response to weight loss is variable; not all individuals have restoration of ovulation or menses despite similar weight reduction. Weight loss results in a decrease in serum androgen concentrations and, in some instances, improvements in hirsutism.
There is no good evidence that one type of diet is superior to another for women with PCOS. Low-carbohydrate diets have become very popular for women with PCOS, based upon the notion that less carbohydrate leads to less hyperinsulinemia and, therefore, less insulin resistance. However, a 12-week study of a high protein/low carbohydrate diet (30% protein, 40% carbohydrate, 30% fat) and a low protein/high carbohydrate diet (15% protein, 55% carbohydrate, 30% fat) were equally effective for weight loss, improvements in menstrual cyclicity, insulin resistance, dyslipidemia, and abdominal fat in one study of 28 overweight women with PCOS. It is unknown if a deficient carbohydrate diet would be more effective for these endpoints.
Yes, it's entirely possible. In fact, in most women, it's recommended that you try naturally first for 6-12 months, depending on your age. Taking Inofolic (myoinositol) – available at most leading chemists - will help you to produce eggs of a 'better quality', ultimately leading to a higher birth rate.
Failing this, we can try clomiphene, an anti-oestrogen used to suppress some of the features of PCOS. Unfortunately, this is associated with a slightly increased risk of multiple pregnancy. It is also associated with a higher pregnancy rate than Inofolic, but Inofolic has a better long-term outcome (higher birth rate).
Endometriosis is defined as endometrial glands and stroma that occur outside the uterine cavity. The lesions are typically located in the pelvis but can occur at multiple sites, including the bowel, diaphragm, and pleural cavity. While endometriosis is a common and nonmalignant process, ectopic endometrial tissue and resultant inflammation can cause painful menstruation, pain during intercourse, chronic pain, and infertility. Symptoms can range from minimal to severely debilitating.